The need for a comprehensive approach - Jenny's case study
Jul 04, 2023Introduction
In the ever-evolving healthcare landscape, traditional models of care, often siloed and reductionist, are being challenged by a surge of evidence from multiple disciplines, each shedding light on the multifaceted nature of health and disease. As health and change professionals, we are at the forefront of a transformative era where a paradigm shift towards a more comprehensive, integrated approach to patient care is not only beneficial, but critical to improving client outcomes, particularly in complex and challenging cases.
This article presents a clinical case that highlights the value and need for such an approach. It illustrates the case of a woman called Jenny, who struggles with the intertwined problems of chronic pain, depression and fatigue, among others. Her story echoes that of many patients around the world who are trapped in a maze of coexisting conditions, struggling to find relief and improvement.
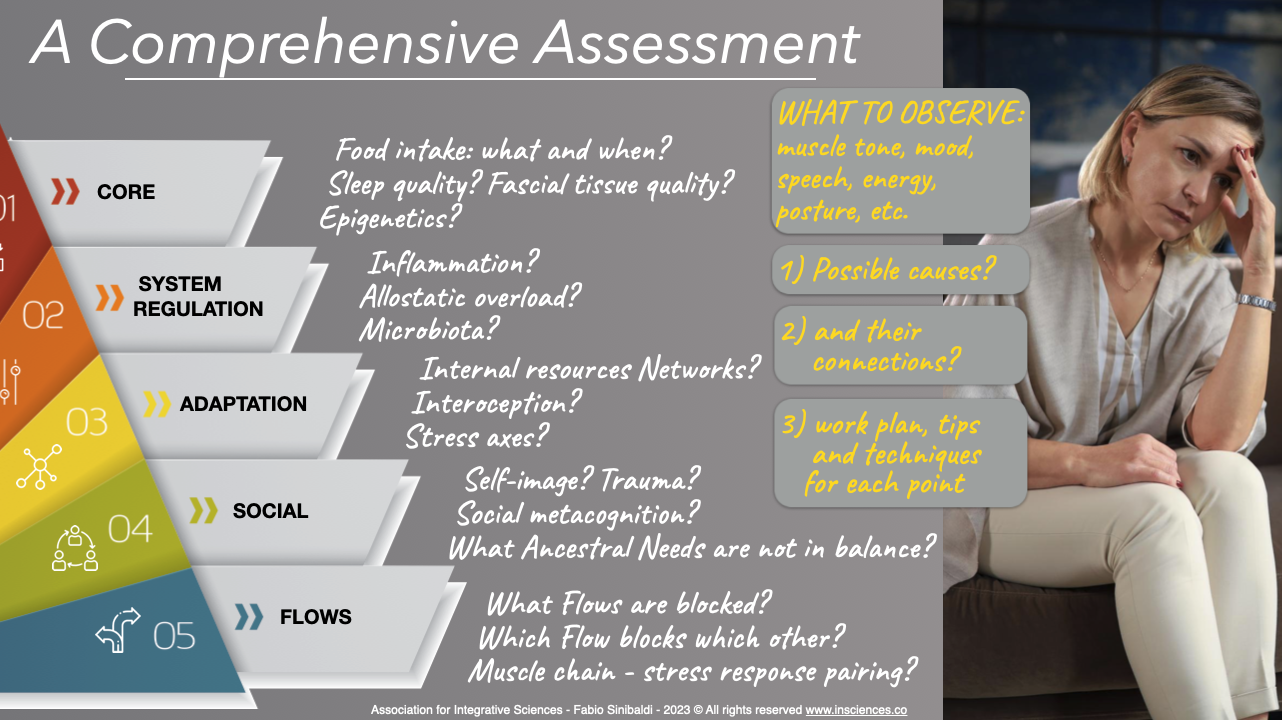
The case highlights the importance of looking at patients like Jenny through a broader, multidimensional lens, incorporating perspectives from different sectors, disciplines and approaches.
Such a comprehensive approach promotes a deeper understanding of the patient's needs, enables the formulation of personalised care strategies, and ensures that the interventions used address not only the apparent symptoms but also the underlying causes at multiple levels.
Focusing on key elements
In this article, we will focus on several selected issues relevant to Jenny's case, rather than attempting to analyse every single aspect involved. This decision reflects a conscious choice to provide depth rather than broadness, to delve deeply into a select number of issues in order to facilitate a thorough understanding, rather than spread ourselves across a wide range of issues. This approach allows us to highlight the complex interplay between different facets of Jenny's physical and mental health, providing a more detailed and nuanced perspective.
We recognise that each symptom and difficulty experienced by Jenny could be explored from a myriad of theories or approaches, each with its own set of insights and implications. However, to present an exhaustive exploration of all these perspectives would result in an overwhelmingly large document, which would likely dilute the focus and detract from our purpose.
Instead, we have chosen to highlight some of the most relevant issues from our integrative perspective. In doing so, we aim to demonstrate the potential richness and depth of an integrative approach, and how it allows us to weave together insights from different disciplines into a coherent, comprehensive understanding of Jenny's health. This approach underscores the value of drawing from different fields and highlights the myriad tools and perspectives that we, as healthcare professionals, can incorporate into our practice to enhance our effectiveness and better serve our patients.
Through this targeted exploration, we hope to inspire you to see the potential of an integrative approach, to appreciate the richness and diversity of insights it can offer, and to consider how you might expand your own practice to more comprehensively address the complex health needs of your clients or patients.
Presenting Problem
Jenny, a 42-year-old woman, presents with symptoms of chronic pain, depression, and fatigue. She mentions a history of high-stress work as a corporate lawyer, and an emotionally abusive relationship in her past. She leads a sedentary lifestyle, often working late hours and skipping meals. Jenny also notes a recent weight gain of approximately 15 kg over the past year and the onset of recurrent digestive problems, including bloating and constipation.
Clinical Observations
Jenny's posture is hunched, suggesting a lack of confidence, other emotional or personal issues, possible musculoskeletal or miofascial problems. Her shoulders are rounded and tense, likely contributing to her reported chronic pain. Her voice is deep and monotonous, with speech patterns indicative of low self-esteem and depressive thinking, including self-blame and expressions of hopelessness. Jenny's skin appears pale, possibly reflecting poor nutrition or chronic stress. She is overweight. She also reports sleep disturbances and poor concentration, often losing the flow of thought during the session.
1 - Mental and Communicative Flows
Jenny's speech patterns and cognitive processes provide insights into her emotional state and needs. Her communication is characterised by a self-deprecating tone and negative conjunctions, indicating a tendency towards self-blame and pessimistic thinking. She frequently uses phrases such as ‘I can’t’, ‘I'm not good enough’ and ‘I always mess up’, painting a picture of someone who sees herself as incapable and undeserving.
Her sentences often contain a high frequency of negative conjunctions such as ‘but’, ‘however’ and ‘although’. These conjunctions may indicate a tendency to dismiss or downplay the positive while emphasising the negative, further reinforcing her depressive cognitive patterns.
From an Integrative Sciences perspective, Jenny's speech and thought patterns are not seen as mere symptoms of an underlying disorder, but as processes that play an active role in her mental health. This perspective allows us to focus on how she constructs her experiences through her language and how these constructions shape her emotional responses and behaviours.
Understanding these patterns opens up a range of potential therapeutic interventions. The Flows and Needs worksheet can be used to first identify and then change these patterns to cultivate a richer repertoire.
We can also use the Mind O' Clock technique (which focuses on the way thoughts flow, regardless of their specific content) to promote greater awareness of her thought flows. Jenny can learn to observe her thoughts without getting caught up in them, thereby reducing their impact on her emotions and behaviour, and redirecting her thinking back into physiological modes that are appropriate to the goal and context.
2 - Postural Flows
Jenny's poor posture and chronic pain could be addressed through Isometric Emotions, Psychosomatic Stretching, Interpersonal Accommodation and other release techniques (you can find them all here). These methods can particularly help to reduce the tension in her muscles as they are the result of various synergistic forces (stress, trauma, poor posture, altered body maps, etc.). We can also work on improving her body alignment, matching her physiology with her identity, self and body maps.
We could also introduce her to the Vagal Reset technique to release unneeded tension and suggest the Resource Balance exercises to strengthen her muscles and sense of mastery (both physical and mental), improve flexibility, increase a sense of stability (both physical and mental) and further reduce pain.
Her hunched posture could be a result of tight myofascial tissue, which could also be contributing to her chronic pain. Our psychosomatic myofascial release techniques could be beneficial in releasing this tension, improving her posture and possibly reducing her pain. In addition, educating Jenny about the role of fascia in maintaining good posture could be a useful part of her overall treatment plan.
3 - Sociality, Attachment and Metacognition
From a social and interpersonal perspective, Jenny's psychological distress can be understood as a result of her difficulties in understanding and managing her own adaptive processes, particularly within interpersonal contexts. These issues manifest in various aspects of her relationships, including power dynamics, attachment and detachment, relational trauma, and emotional regulation during social interactions.
Jenny's history of an emotionally abusive couple may have led to an imbalance of power in the relationships. She appears to have internalised a sense of powerlessness and often complies with the demands made by others at the expense of her own needs. Her language and signals of Interpersonal Accommodation reflect a submissive role, suggesting a habit of putting others before herself, possibly to avoid conflict or rejection.
Jenny may oscillate between an intense desire for closeness and a fear of being hurt, leading her to withdraw emotionally from relationships. This pattern could contribute to a cycle of unstable relationships, reinforcing her feelings of worthlessness and despair. We can help her to develop functional ways of being attached or detached.
Her history of an emotionally abusive relationship also points to relational trauma. Such trauma can lead to difficulties in trusting others and a heightened sensitivity to potential threats in interpersonal situations. This could lead her to misinterpret the behaviour of others, perceive benign actions as threatening and react with disproportionate emotional responses. Interestingly, these processes are also mediated by an excess of glutamate in the brain and an altered gut microbiome. In any case, we need to restore a physiological state and support her to find new ways of developing interpersonal trust, for example using the tools offered by the Evolutionary Relationship Approach. For instance, to address power imbalances, the therapist could help Jenny to recognise her submissive patterns and explore their roots from a neuro-ethological perspective. They could then work together to develop strategies for gradually shifting the power dynamics.
In terms of emotional regulation in social interactions, Jenny may struggle with poor timing in managing her emotional-relational responses. For example, she might suppress her feelings when it would be effective to express them (e.g. to get help or to strengthen a relationship) or become overly emotional and aggressive in situations where it takes time to understand what is happening and what the other person's real intentions are. This could further complicate her interpersonal relationships, leading to misunderstandings and conflicts.
4 - Emotions and Brain Networks
To help Jenny, we need to focus on her emotional experiences and her ability to use emotions adaptively. The therapist would help Jenny to become more aware of her emotional responses, to understand where they come from and to use this information to inform her decision-making. This could help Jenny to manage her depressive symptoms and improve her overall emotional health.
A modern science-based theory of constructed emotions could provide insights into how Jenny's emotions are influenced by her past experiences, expectations, predictions, and current context. This perspective could help Jenny to understand and manage her emotional responses more effectively and provide her with tools such as the Parallel Worlds and Possible Scenarios to counter her predictive system.
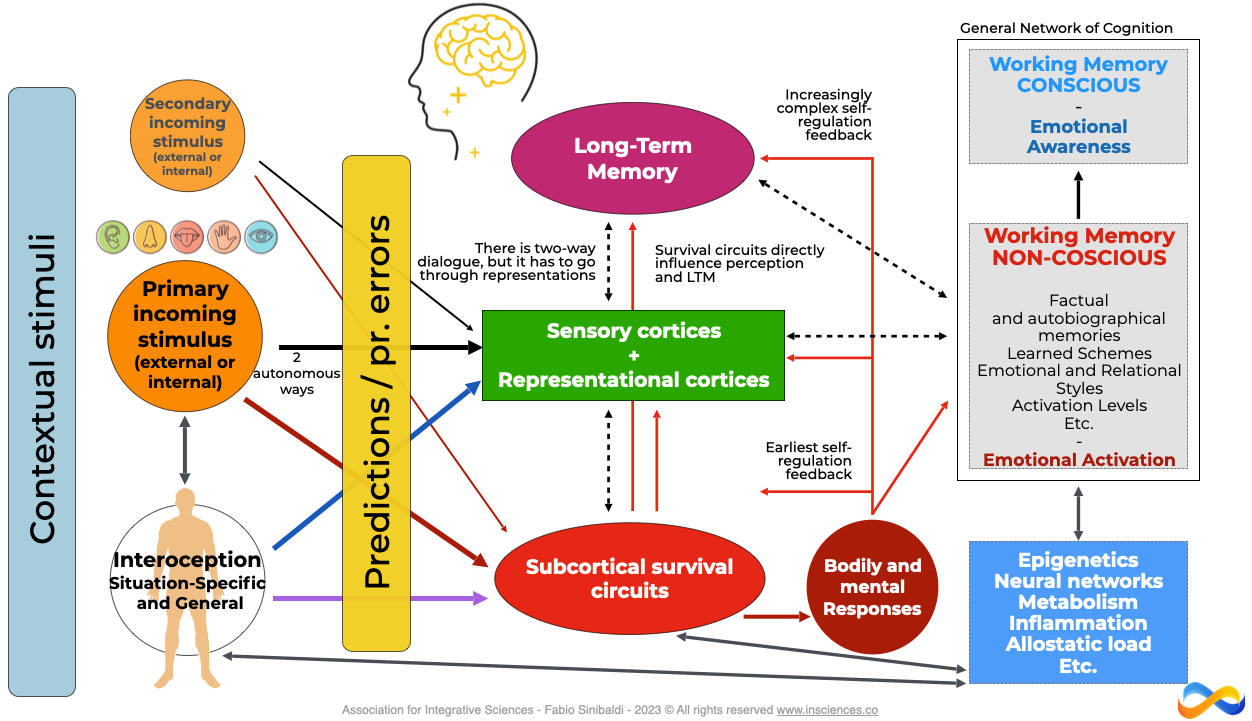
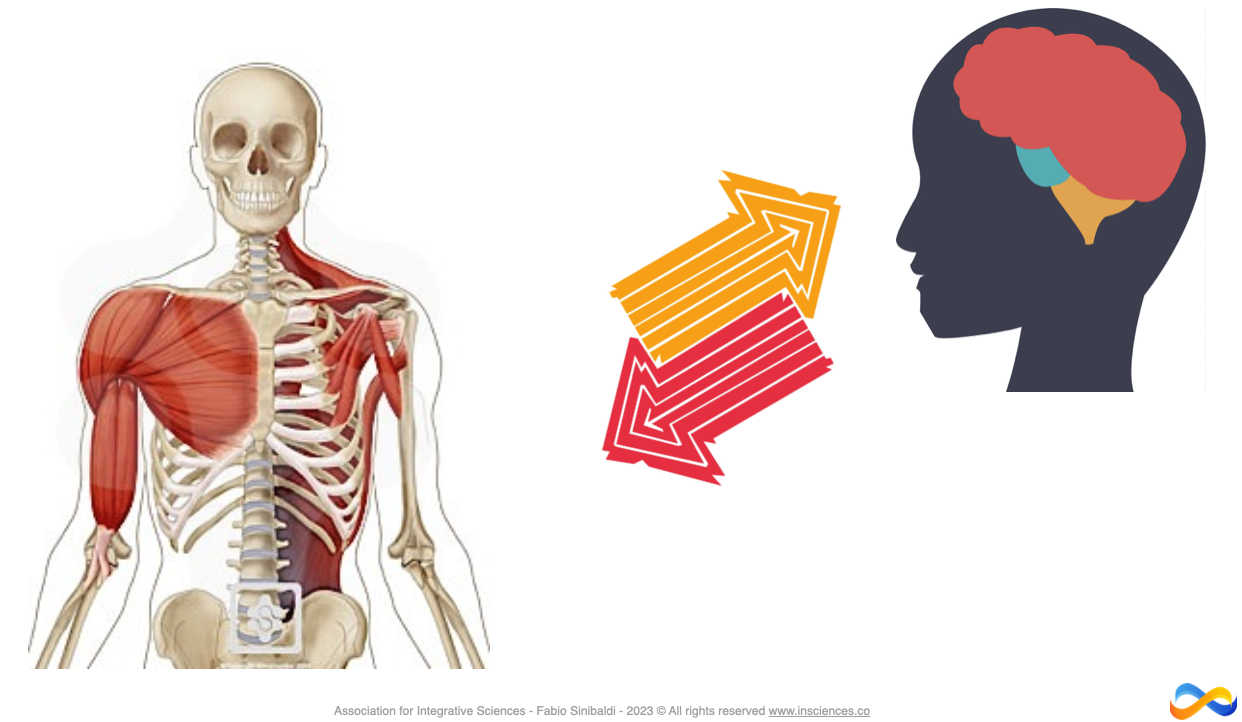
From a neuroscience perspective, Jenny's depression may be related to altered brain function, including changes in areas responsible for emotion regulation such as the Salience Network (including the amygdala, the insular cortex and other strategic neural nodes). In particular, Jenny's chronic stress and emotional trauma may have affected her autonomic nervous system, contributing to her symptoms.
Understanding these aspects could inform therapeutic interventions such as Integrative Mindfulness practices, Integrative Functional Patterns, Emotion & Behaviour Modulation with Post-its to improve emotional regulation and interpersonal functioning.
We can also use Isometric Emotions and other techniques to help Jenny develop awareness of her bodily sensations and how they relate to her emotions, to help her manage her chronic pain and improve her emotional regulation.
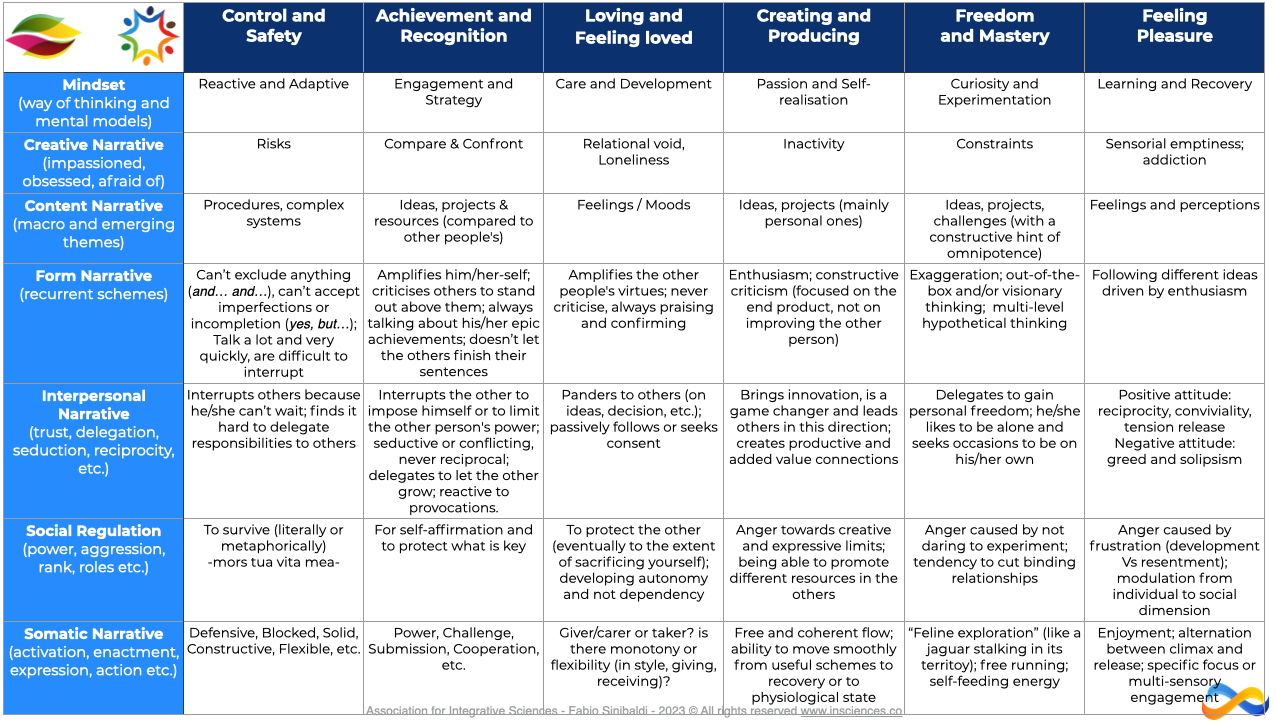
5 - Motivations and Needs
Understanding Jenny's motivations and needs can guide her treatment. For instance, if Jenny is motivated to improve her physical health and regain control of her life, this can be a strong driving force in her therapy and lifestyle changes. Identifying her needs, such as the need for control and safety, for physical activity, for freedom of choice, can also inform the treatment approach.
Understanding motivations and needs is a complex task that is often oversimplified in traditional models. Rather than a linear, hierarchical structure, as often depicted in models such as Maslow's hierarchy of needs, motivations and needs are better represented as a complex, non-linear network of influences, with many interconnections and interdependencies. This perspective recognises the multifaceted and dynamic nature of human motivation, taking into account physiological, psychological, ethological, relational, epigenetic and environmental factors.
In Jenny's case, her motivations and needs may be intertwined in complex ways that contribute to her current challenges. For example, her need for emotional safety may conflict with her desire for close relationships, given her history of an emotionally abusive relationship. This conflict could motivate behaviour that seems contradictory, such as seeking closeness while pushing people away, leading to unstable relationships. Furthermore, the physical pain may act as a form of protection, preventing her from engaging in activities or relationships that might threaten her emotional safety. Indeed, Jenny may also experience resistance to change. Although she wants to improve her mental and physical health, part of her may resist the changes needed to achieve this.
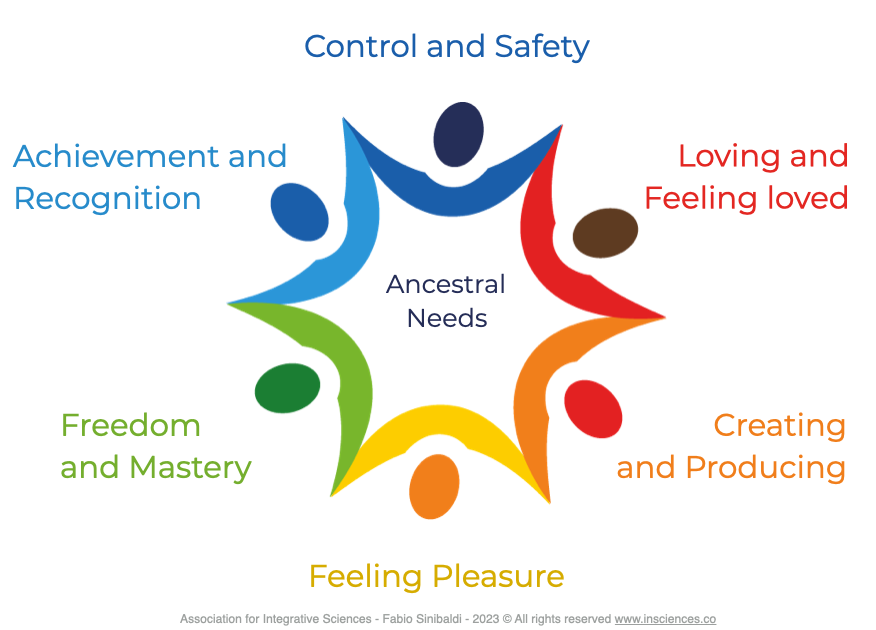
Importantly, if our needs are not adequately met over a long period of time, this can lead to the development of psychosomatic disorders. The mind-body connection is powerful, and unfulfilled emotional needs can manifest as physical symptoms. In Jenny's case, her chronic pain and fatigue could be seen as psychosomatic responses to unmet needs, such as the need for safety, autonomy or self-worth. From this perspective, her chronic pain could reflect a state of multiple needs that have been unrealised for long periods of time.
Addressing these needs and motivations could involve various therapeutic interventions. For example, the therapist might help Jenny to identify her conflicting needs and explore ways of balancing them. They might even explore fears about a particular need that might be contributing to her resistance to change. In general, understanding Jenny's motivations and needs provides important insights into her experiences and behaviours. By addressing these needs in a more integrated and targeted way, we can help her to manage her conflicts, overcome her resistance and promote a healthier mind-body integration, thereby promoting her overall wellbeing.
6 - Inflammation, Nutrition and Allostatic overload
Jenny's conditions can be viewed through the lens of the interconnectedness of mental health and metabolic processes. Integrative Sciences emphasise the importance of metabolic health in mental wellbeing, bridging the gap between psychiatry, endocrinology and nutritional science.
Jenny's chronic pain, fatigue and depressive symptoms may be related to underlying metabolic dysregulation. For example, chronic inflammation, often associated with metabolic syndrome, can affect brain function and mood, contributing to symptoms of depression. In addition, poor diet and gut health can affect the production and regulation of neurotransmitters such as serotonin and dopamine, which play a key role in mood regulation and cognitive function.
On the other hand, her mental health issues may also contribute to metabolic dysregulation. Chronic stress and depression can affect hormonal balance, alter gut microbiota, and lead to unhealthy lifestyle choices such as poor diet and physical inactivity, further exacerbating metabolic dysfunction.
When looking at the metabolism of the mind, we need to consider the energy and nutrient needs of the brain. Jenny's symptoms of fatigue and cognitive difficulties may reflect an energy imbalance in her brain. Poor diet, physical inactivity and chronic stress can impair the brain's ability to produce and use energy efficiently, affecting cognitive function and mood regulation.
Addressing these metabolic aspects of Jenny's treatment could include interventions such as dietary changes, physical activity, sleep-wake cycles, stress management techniques, and eventually the use of dietary supplements or medications to target specific metabolic dysfunctions. By improving her metabolic health, we can positively influence her brain function and mental health, providing a more comprehensive and integrative approach to her care.
Conclusion
By integrating many different perspectives, we recognise the inherent interconnectedness of the human system. Every layer of our being, from our physiological processes to our cognitive patterns, from our genetic make-up to our lived experiences, is inextricably linked, influencing and being influenced by each other. This understanding requires a shift from traditional, compartmentalised treatment strategies to a more integrated and integrative approach.
This article is a call to action for all health professionals to embrace this integrated approach, to venture beyond their specialties and to appreciate the vast, interconnected landscape of human health. It is an invitation to cultivate a spirit of curiosity and lifelong learning, to continually broaden our horizons and deepen our understanding of the patients or clients we serve. It is a demonstration of the power of the strength of a multidisciplinary approach and the profound impact it can have on improving patient outcomes.
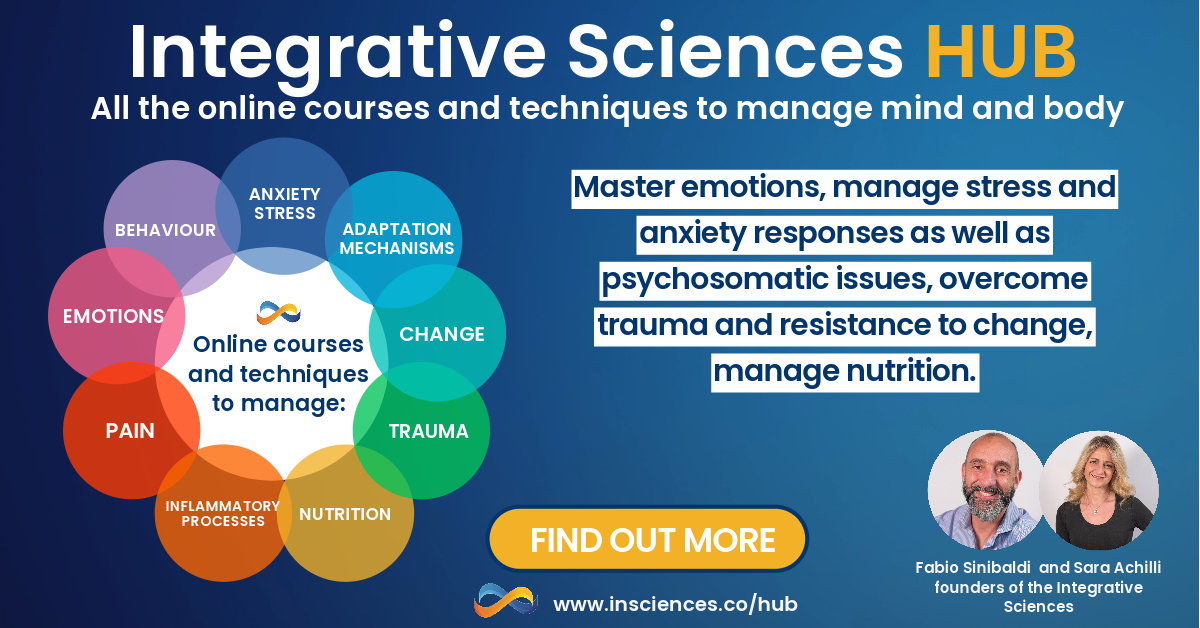
Do you want to find out more?
Discover the many online courses on psychosomatic processes, regulation of anxiety and stress responses, emotion modulation, trauma and resistance to change. They are all part of the Integrative Sciences HUB, our regularly updated online training centre, available to you 24/7 with new COURSES, UPDATES, TECHNIQUES AND PRACTICAL TOOLS each month.
Stay connected with news and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.
We hate SPAM. We will never sell your information, for any reason.